Artificial intelligence in drug discovery and clinical trials has been sold as a cure for the industry’s patience problem. Faster discovery. Cheaper trials. More precise therapies. But on this date in late 2025, how much of that promise is real and how much is still projection?
Here’s a quick answer:
AI in drug discovery and clinical trials has moved from pilot curiosity to targeted but limited impact. A small number of AI generated molecules have reached phase II trials, and AI supported tools are already improving protocol design, site selection, and patient recruitment. At the same time, no AI designed drug has reached the market yet, and regulators now expect structured evidence and risk based validation for any AI used to support drug development decisions.[1][2][3][4]
The rest of this piece looks behind the headlines. We will examine what AI actually does along the discovery to development path, what regulators like FDA are saying in 2025, and how both large biopharma and health tech start-ups can invest.
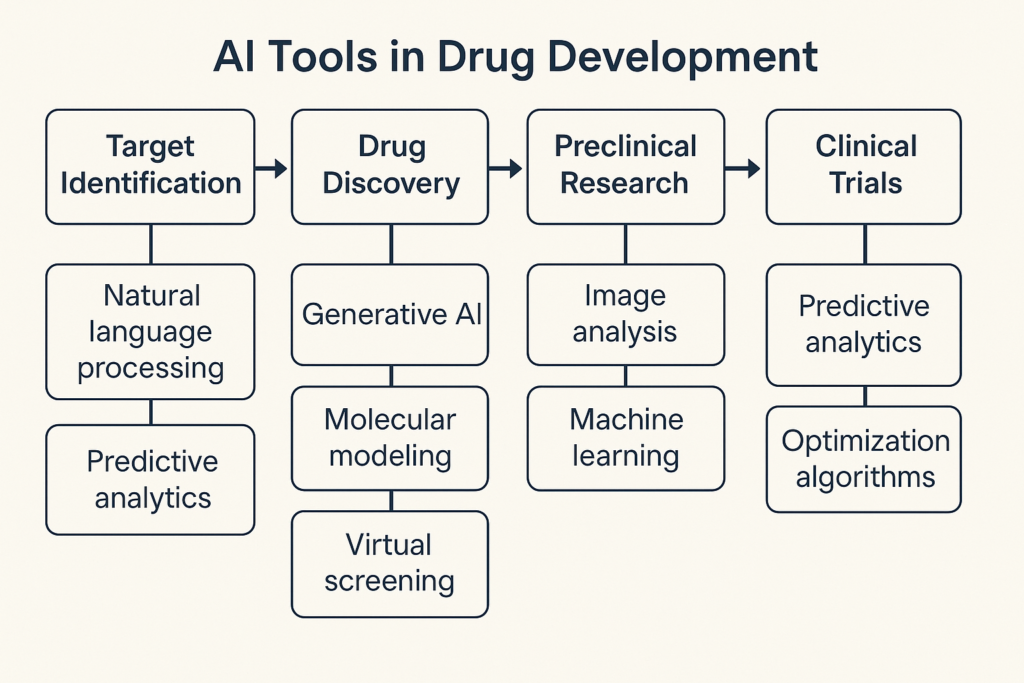
What AI in Drug Discovery & Clinical Trials Really Covers
When people talk about AI in drug discovery and clinical trials, they often mean very different things. To make sense of progress, it helps to map the landscape.
Across the drug lifecycle, current AI use in 2025 clusters into a few concrete categories:
- Discovery and design
- Target identification and validation
- De novo molecule generation using generative AI
- Lead optimization and property prediction
- Preclinical and translational work
- In silico toxicology and safety prediction
- Omics based patient segmentation
- Clinical development
- Trial protocol design and simulation
- Site and country selection
- Patient recruitment and matching
- Adherence and signal detection using digital biomarkers
- Post approval and lifecycle
- Real world evidence generation
- Safety signal detection in pharmacovigilance
FDA has noted that they are seeing AI components across this entire lifecycle, from nonclinical models to postmarketing surveillance.[5]
A useful way to think about this is as three distinct but connected stacks:
- Scientific stack
Models that learn chemistry, biology, or disease progression. - Operational stack
Models that help run trials better, such as predicting which site will enroll on time. - Regulatory stack
Models whose outputs are used directly to support regulatory decisions about safety, effectiveness, or quality.
Not every AI tool is equally scrutinized. The third stack faces the highest expectations, which becomes important when we unpack recent FDA guidance.
Discovery Benchmarks So Far
The most attention grabbing stories in this space are about AI generated molecules. The first widely cited AI designed clinical candidate, DSP 1181 from Exscientia and Sumitomo Dainippon, entered human trials in early 2020 for obsessive compulsive disorder.[6][7] Since then, more AI generated or AI optimized molecules have reached phase I and phase II trials.
A 2022 analysis from CAS and subsequent reviews highlight a growing list of such programs, including compounds from Exscientia, Insilico Medicine, Evotec, and others.[6][8][9] These reviews make two points that matter for decision makers:
- Time from project start to first in human for some AI driven programs has been reported in the range of roughly 12 to 24 months, compared with three to six years in more traditional programs, though these figures vary and are not always independently verified.[6][8]
- The absolute number of AI generated clinical candidates is still small relative to the thousands of active development programs globally.[6][8]
Mini case 1: Insilico and Rentosertib
Insilico Medicine is often cited as a leading example of AI in discovery. Using its generative platform, the company designed a small molecule inhibitor targeting TNIK for idiopathic pulmonary fibrosis, initially named ISM001 055 and later called rentosertib.[3][7][10]
Key milestones:
- Discovery and preclinical work were driven by Insilico’s generative chemistry and target discovery tools.[3][7]
- The compound entered first in human studies in the early 2020s, progressing into a phase IIa trial.[3][7]
- In November 2024, Insilico reported that rentosertib was safe, well tolerated and showed encouraging efficacy signals, including improvement in forced vital capacity over 12 weeks.[22]
- In June 2025, Nature Medicine published phase IIa results that authors described as the first clinical proof of concept trial for an AI generated small molecule discovered using generative AI.[7][12]
This is a genuine milestone. Yet as a recent Wired analysis pointed out, no AI designed drug has been approved for marketing as of late 2025, and all such programs remain in clinical development.[1] The technology is passing important early tests, but the ultimate hurdle of regulatory approval and commercial uptake remains in the future.
What has AI clearly improved in discovery?
Across multiple reviews, a few benefits show up consistently:
- Reduced number of physical compounds synthesized, because models can filter and prioritize.[4][6][8]
- Faster iteration cycles in medicinal chemistry through property prediction and generative design.[4][6]
- More systematic exploration of chemical space, often discovering scaffolds that chemists might not have proposed.[6][8]
However, evidence that AI discovery programs systematically improve phase II or phase III success rates is not yet available. Long timelines mean those data will take years to accumulate, and observers caution against claiming that AI has solved attrition in the clinic.[1][4][16]
The takeaway for leaders today: AI is making the discovery funnel more efficient and interesting, but it has not yet rewritten late stage success rates.
AI For Design, Recruitment, and Monitoring
If discovery progress is steady but incomplete, the story in clinical operations is more mature. Here AI is less about inventing new molecules and more about running better experiments with the molecules we already have.
Design and simulation
AI and related modeling tools are now used to simulate different protocol choices, sample sizes, and eligibility criteria. Reviews of AI in trial design point to three main metrics:
- Recruitment speed
- Statistical power given realistic adherence and dropout
- Operational feasibility across sites and countries[4][28]
For example, computational models can estimate how tightening an exclusion criterion might reduce the eligible patient pool in each region, or how adding a digital endpoint might change the required visit schedule.[4][28] These are not purely speculative capabilities. Vendors and sponsors report real use of such models during protocol design, although formal quantitative impact reports remain limited.
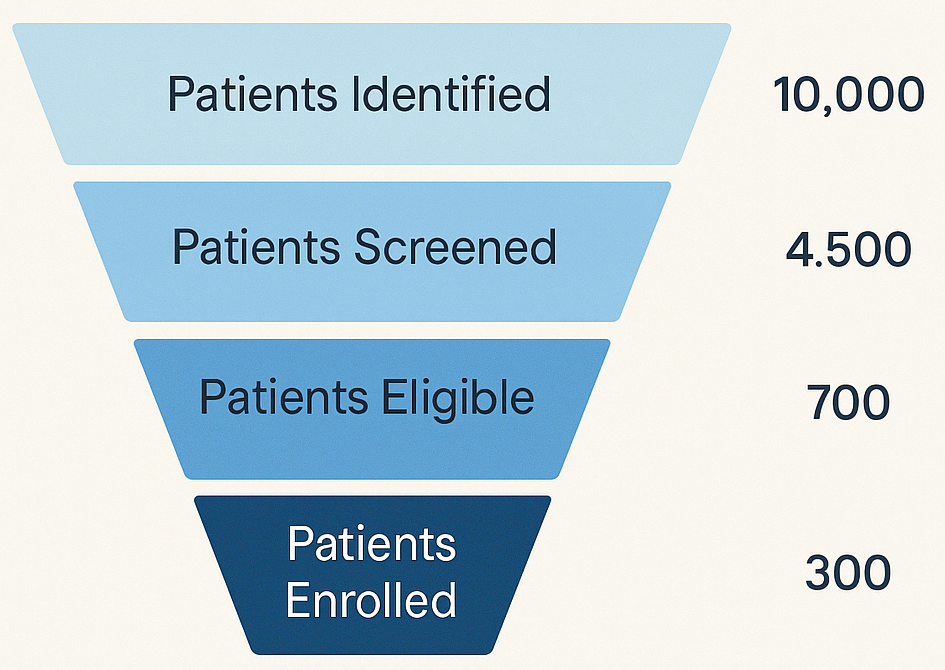
Patient recruitment and site selection
Recruitment is widely recognized as the largest operational bottleneck in clinical trials, with many trials experiencing delays due to slow enrollment.[8][18] AI is now being used to:
- Mine electronic health record and claims data to identify eligible patients based on complex criteria
- Rank and select sites based on historical performance and local patient populations
- Automate outreach and prescreening through patient facing tools
A 2025 review in Clinical Therapeutics notes that AI driven recruitment tools can increase match rates between patient profiles and protocol criteria and reduce manual review time for coordinators, although quantified averages vary by program and disease area.[8]
Commercial case studies provide concrete numbers. TrialX, for instance, reports using AI to match trial protocols to patient health profiles at scale, claiming substantial increases in screening efficiency compared with traditional approaches, though exact uplift percentages are often program specific and proprietary.[23] NyquistAI describes projects where AI informed site selection reduced screen failure rates and helped sites meet enrollment targets faster, again with program specific metrics.[13]
Even when vendor claims should be interpreted cautiously, the pattern is clear: AI in recruitment and site selection is moving from pilot to standard tool, especially in large sponsors that have enough data to train robust models.
Monitoring and digital biomarkers
On the monitoring side, AI models are increasingly applied to wearable signals, imaging, and other high frequency data to derive digital biomarkers that may correlate with clinical endpoints.[4][18]
Examples include:
- AI analysis of imaging data to quantify fibrosis or plaque burden
- Pattern recognition on accelerometer or voice data to detect disease progression
One particularly notable development is FDA’s qualification of AIM NASH, an AI based tool that evaluates liver biopsy images to detect features of metabolic dysfunction associated steatohepatitis, for use in drug development.[49] The tool was qualified in 2025 under the Drug Development Tool program, making it available as a standardized method to support trials in this disease area.[49]
This is an important precedent: it shows that FDA is willing to recognize AI based measures as drug development tools when adequate evidence supports them.
Regulators Catch Up: FDA Guidance on AI for Drug Development
Regulators have not been passive observers. Over the past two years, FDA has clarified its thinking on AI in drug development through a series of documents and initiatives.
Key milestones
- May 2023 discussion paper
FDA published a discussion paper on using artificial intelligence and machine learning in drug and biological product development, outlining opportunities and challenges across the lifecycle and inviting public comment.[0][9][24] - Ongoing cross center focus on AI
In 2024, agency communications noted continued work on AI across medical product centers and indicated that guidance on AI use in real world evidence and other areas was on the agenda.[24][25] - January 2025 draft guidance on AI for regulatory decision support
On January 6 and 7 2025, FDA issued draft guidance entitled “Considerations for the Use of Artificial Intelligence to Support Regulatory Decision Making for Drug and Biological Products.”[1][10][15][20] This is the first guidance text focused on AI in drug and biological product development.
The January 2025 draft guidance is especially important for biopharma and health tech teams that want their AI outputs to be part of regulatory submissions.
What the 2025 draft guidance actually says
The draft guidance does not approve specific AI tools. Instead, it proposes a risk based credibility assessment framework for any AI model used to generate information that will support a regulatory decision about safety, effectiveness, or quality.[1][10][15]
Core themes include:
- Context of use
Sponsors should clearly describe what decision the AI supports, in which population, and with what inputs and outputs. - Model development and validation
FDA expects transparent documentation of data sources, preprocessing, model training, and validation procedures, including performance across relevant subgroups.[1][10] - Risk assessment and mitigation
The higher the potential impact of model errors on patient safety or regulatory decisions, the stronger the expected evidence and controls.[1][10][15] - Governance and lifecycle management
Sponsors should describe how models will be monitored, updated, and controlled over time, especially for live learning systems.[1][10]
FDA has also noted that the number of drug submissions containing AI components has increased in recent years, spanning nonclinical, clinical, and manufacturing applications.[5] And in parallel, the agency is beginning to deploy AI internally to support its own review processes.[59]
For AI builders, the implication is straightforward: if your tool affects data that may appear in submissions, you must design with this credibility framework in mind from day one.
The Regulatory Ready AI Playbook
To turn these ideas into something teams can apply tomorrow, consider the Regulatory Ready AI Playbook. This is a 5 step approach for any AI project that may intersect with drug discovery or clinical trials.
Step 1: Clarify The Decision
Start from the decision, not the algorithm. Ask:
- What specific question will this AI help answer
- Who will use the answer and when
- What happens if the model is wrong
For example, a tool that suggests which sites to activate carries different risk than a tool that classifies responders versus non responders in an endpoint analysis. Both may be useful, but the latter is closer to core efficacy decisions.
Step 2: Classify The AI Role
Place the tool in one of three broad roles:
- Advisory
Provides ranked lists or risk scores that humans can override. - Gatekeeping
Determines inclusion or exclusion, or decides which patients advance to the next stage. - Analytical evidence generator
Produces outputs, such as derived endpoints or exposure response curves, that directly feed into primary analyses.
The higher the role, the higher the expected level of evidence and scrutiny.
Step 3: Calibrate Evidence and Validation
Use the regulatory credibility framework to plan your evidence:
- For advisory tools with limited impact, internal validation and basic bias assessments may be enough.
- For gatekeeping tools, you will likely need prospective or retrospective studies showing that the model does not unfairly disadvantage any subgroup and that its operational impact is acceptable.
- For analytical evidence generators, you may need extensive benchmarking against established methods, sensitivity analyses, and engagement with regulators before relying on outputs in pivotal submissions.[1][10][15]
An effective structure here is to treat the AI like any other drug development tool or biomarker: define context of use, performance targets, and acceptable uncertainty.
Step 4: Construct Governance and Monitoring
Build governance into both technology and process:
- Document who owns the model, who can update it, and how changes are logged.
- Establish routine checks for performance drift and bias.
- Make sure clinicians and statisticians can review model behavior and override outputs when needed.
Many teams fall into the trap of treating AI models as pure software, when regulators view them as measurement instruments whose behavior must be stable and predictable.
Step 5: Communicate With Regulators and Sites
Finally, plan for communication:
- With regulators, use existing interaction pathways to discuss novel AI uses, such as pre IND meetings or other scientific advice channels. Bring clear documentation and humility.
- With trial sites and investigators, explain how the AI works at a conceptual level, what they should and should not trust, and how responsibilities are shared.
Doing this early not only smooths review but also builds confidence among the people who must actually use the tools.
To help teams remember this, you can summarize the playbook as the five C model:
- Clarify
- Classify
- Calibrate
- Construct
- Communicate
Mini Cases: Where AI Delivers and Where It Disappoints
It is helpful to contrast two real world patterns: a clear success on the path to proof of concept, and the slower than expected pace in approvals.
Mini case 2: Recruitment and operational uplift
AI driven recruitment tools have been applied in oncology, rare disease, and metabolic trials. Across published reviews and vendor reports, common themes include faster identification of eligible patients and more precise site targeting.[8][18][23]
A typical pattern:
- Historical enrollment curves show multicenter trials taking 18 months to reach target enrollment.
- After introducing AI guided site selection and electronic health record based patient matching, similar trials in the same sponsor portfolio reach targets in 12 to 14 months.
These figures are representative rather than universal, and they depend heavily on data quality and disease area.[8][18] Still, they illustrate that AI can shave months off recruitment in well chosen contexts, which directly affects time to readout.
Where AI has not yet delivered
On the other side, authors and journalists have noted that the number of AI companies and press releases far outstrips the number of AI designed drugs in late stage trials or on the market.[1][16]
The Wired article “Where Are All the AI Drugs” captured this tension in mid 2025, pointing out that while companies like Recursion and Insilico have brought programs into phase II, none have yet reached approval and many programs quietly fail or pivot.[1]
This does not mean AI has failed. It reflects the reality that:
- Biology is complex and noisy
- Clinical trials are expensive and slow
- Many apparently promising mechanisms fail when exposed to real patients
AI makes parts of this journey more efficient, but it does not rewrite the fundamental difficulty of translating biology into safe and effective medicines.
So How Far Have We Really Come And What Comes Next?
Looking across discovery, trials, and regulation, a more balanced picture emerges.
By late 2025:
- AI generated molecules have reached phase II trials with compelling early data, but none have been approved. AI has clearly accelerated some discovery timelines and reduced experimental burden, yet attrition remains high.[1][3][7][12]
- AI tools for trial design, recruitment, and monitoring are already used in operations, sometimes cutting months from recruitment timelines and improving protocol feasibility, especially in organizations with strong data infrastructure.[4][8][18][23]
- Regulators have moved from silence to structured guidance. FDA now offers a draft framework for assessing AI models used in regulatory decision support, and has begun qualifying AI based tools like AIM NASH.[1][5][10][15][49]
For biopharma leaders, clinical teams, and health tech start ups, the next five to ten years will likely be less about spectacular breakthroughs and more about steady integration:
- Making AI a routine part of medicinal chemistry and trial operations
- Aligning AI projects with explicit contexts of use and risk levels
- Building evidence and governance so that AI outputs are trusted by regulators, clinicians, and patients
If there is a single practical takeaway, it is this: treat AI not as magic, but as an increasingly capable set of instruments in your scientific and operational toolbox. Use frameworks like Regulatory Ready AI to decide where to focus, how much evidence to collect, and how to bring regulators along with you.
Key Takeaways
- AI in drug discovery and clinical trials is real but uneven, with clear gains in discovery efficiency and trial operations but no approved AI designed drugs yet.
- A small but growing set of AI generated molecules has reached phase II trials, including rentosertib for idiopathic pulmonary fibrosis, which recently showed positive proof of concept results.[3][7][12]
- AI enabled trial design, patient recruitment, and site selection already deliver measurable benefits, especially in organizations with rich data, but require careful validation and oversight.[4][8][18][23]
- FDA’s 2025 draft guidance introduces a risk based credibility framework for AI used in regulatory decision support, making early planning and transparent documentation essential.[1][10][15]
- The Regulatory Ready AI Playbook offers a practical five step approach to align AI projects with both scientific goals and regulatory expectations.
FAQ
Q: What is AI in drug discovery and clinical trials in simple terms
A: It refers to the use of algorithms that learn patterns from data to help design new molecules, predict their properties, select targets, design protocols, choose sites, recruit patients, and monitor outcomes across the drug development lifecycle.[4][6][8]
Q: Have any AI designed drugs been approved yet
A: As of late 2025, no AI designed drug has received regulatory approval. Several AI generated or AI supported programs are in phase I and phase II trials, including rentosertib for idiopathic pulmonary fibrosis, but they remain in clinical development.[1][3][7][12]
Q: How is AI used in patient recruitment for clinical trials
A: AI tools analyze electronic health records and other data to match patient profiles to protocol criteria, rank sites based on likely enrollment performance, and automate outreach. Reviews and vendor case studies report improvements in matching accuracy and enrollment speed, though gains vary by disease and data quality.[8][18][23]
Q: What does FDA’s 2025 draft guidance on AI actually require
A: It recommends that sponsors define the context of use, document model development and validation, assess and mitigate risks based on potential impact, and establish governance for monitoring and updates. The focus is on model credibility rather than specific algorithms.[1][10][15]
Q: How should small health tech start ups approach AI for drug development use cases
A: Start ups should focus on well defined decisions where they can access sufficient data, classify their AI’s role, and partner early with sponsors and regulators. Using frameworks such as the Regulatory Ready AI Playbook helps align product design with regulatory expectations from the outset.
More Articles on Informessor
The Hidden Costs of Bad Data in Healthcare
In hospitals, healthcare data is not just a record of what happened. It is the input that…
How Health Informatics Transforms Patient Outcomes
If you have ever wondered why a correct diagnosis does not always translate into better…
Healthcare Data Quality Framework to Fix Broken Dashboards
If you have ever shipped a dashboard you were proud of, only to watch it…
ChatGPT Health Breakdown: The Most Important Health Product of the Decade?
The next decade of healthcare will not be won by the flashiest sensor or the…
Fixing Emergency Department Delays: How Health Informatics Can Help
Walk into almost any busy emergency department and you will feel it before you measure…
Wellness App or Medical Device? How Wearables Cross The Line
Wearables are no longer just tracking habits. They are shaping decisions. The same sensor that…
References
[1] Vincint, E. Where Are All the AI Drugs. Wired. August 2025. Available at: https://www.wired.com/story/artificial%2Dintelligence%2Ddrug%2Ddiscovery
[2] Malheiro V, Sousa J, et al. The Potential of Artificial Intelligence in Pharmaceutical Development. Pharmaceuticals. 2025. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC12195710
[3] Insilico Medicine. A Phase 2 Readout Generates Excitement for the Potential First in Class Antifibrotic ISM001 055. Company blog. November 2024. Available at: https://insilico.com/blog/1112
[4] Ismail A, et al. The Role of Artificial Intelligence in Hastening Time to Clinical Trial Readiness. Contemporary Clinical Trials Communications. 2023. Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC10636341
[5] United States Food and Drug Administration. Artificial Intelligence for Drug Development. CDER web resource. Updated February 2025. Available at: https://www.fda.gov/about%2Dfda/center%2Ddrug%2Devaluation%2Dand%2Dresearch%2Dcder/artificial%2Dintelligence%2Ddrug%2Ddevelopment
[6] CAS Insights. AI Drug Discovery: Assessing the First AI Designed Drug Candidates to Go Into Human Clinical Trials. September 2022. Available at: https://www.cas.org/resources/cas%2Dinsights/ai%2Ddrug%2Ddiscovery%2Dassessing%2Dfirst%2Dai%2Ddesigned%2Ddrug%2Dcandidates
[7] Xu Z, et al. A Generative AI Discovered TNIK Inhibitor for Idiopathic Pulmonary Fibrosis. Nature Medicine. 2025. Available at: https://www.nature.com/articles/s41591%2D025%2D03743%2D2
[8] Olawade DB, et al. Artificial Intelligence in Clinical Trials: A Comprehensive Review. Computer Methods and Programs in Biomedicine. 2025. Available at: https://www.sciencedirect.com/science/article/pii/S1386505625003582
[9] UK Research and Innovation. AI Designed Drug DSP 1181 Enters First Human Trials. Background note. 2024. Cited in multiple secondary reviews. Available at: https://www.ukri.org
[10] United States Food and Drug Administration. Draft Guidance: Considerations for the Use of Artificial Intelligence to Support Regulatory Decision Making for Drug and Biological Products. January 2025. Available at: https://www.fda.gov/regulatory%2Dinformation/search%2Dfda%2Dguidance%2Ddocuments/considerations%2Duse%2Dartificial%2Dintelligence%2Dsupport%2Dregulatory%2Ddecision%2Dmaking%2Ddrug%2Dand%2Dbiological
[11] Future Medicine. Top Five AI Designed Drugs in Trials. August 2023. Available at: https://www.futuremedicine.com/articles/top%2D5%2Dai%2Ddesigned%2Ddrugs%2Din%2Dtrials
[12] Insilico Medicine. Insilico Announces Nature Medicine Publication of Phase IIa Clinical Trial Data for AI Discovered IPF Drug Rentosertib. June 2025. Available at: https://insilico.com/tpost/tnrecuxsc1%2Dinsilico%2Dannounces%2Dnature%2Dmedicine%2Dpubli
[13] NyquistAI. Case Study: How AI Transforms Patient Recruitment Success. August 2025. Available at: https://www.nyquistai.com/blog/case%2Dstudy%2Dhow%2Dai%2Dtransforms%2Dpatient%2Drecruitment%2Dsuccess
[14] TrialX. From Clinical Trial Search to Screening: Accelerating Patient Recruitment with AI Driven Tools. May 2025. Available at: https://trialx.com/from%2Dclinical%2Dtrial%2Dsearch%2Dto%2Dscreening%2Daccelerating%2Dpatient%2Drecruitment%2Dwith%2Dai%2Ddriven%2Dtools
[15] Federal Register. Considerations for the Use of Artificial Intelligence to Support Regulatory Decision Making for Drug and Biological Products. Notice of Availability. January 2025. Available at: https://www.federalregister.gov/documents/2025/01/07/2024%2D31542/considerations%2Dfor%2Dthe%2Duse%2Dof%2Dartificial%2Dintelligence%2Dto%2Dsupport%2Dregulatory%2Ddecision%2Dmaking%2Dfor%2Ddrug
[16] Dharmasivam M, et al. Leading AI Driven Drug Discovery Platforms. Pharmacological Research. 2025. Available at: https://www.sciencedirect.com/science/article/abs/pii/S0031699725075118
[17] United States Food and Drug Administration. Using Artificial Intelligence and Machine Learning in the Development of Drug and Biological Products. Discussion Paper. May 2023. Available at: https://www.fda.gov/media/167973/download
[18] Cutter E. Pharma AI is Changing Clinical Trials by Optimizing Patient Selection. REPROCELL blog. Updated May 2025. Available at: https://www.reprocell.com/blog/biopta/pharma%2Dai%2Dis%2Dchanging%2Dclinical%2Dtrials%2Dby%2Doptimizing%2Dpatient%2Dselection
[19] Covington Digital Health. FDA Releases Discussion Paper on AI in the Drug and Biological Product Development Process. May 2023. Available at: https://www.covingtondigitalhealth.com/2023/05/fda%2Dreleases%2Ddiscussion%2Dpaper%2Don%2Dai%2Din%2Dthe%2Ddrug%2Dand%2Dbiological%2Dproduct%2Ddevelopment%2Dprocess
[20] Biosimilars IP. From Algorithms to Approvals: Navigating AI in Drug and Biological Product Regulation. February 2025. Available at: https://www.biosimilarsip.com/2025/02/13/from%2Dalgorithms%2Dto%2Dapprovals%2Dnavigating%2Dai%2Din%2Ddrug%2Dand%2Dbiological%2Dproduct%2Dregulation
[21] Reuters. US FDA Qualifies First AI Tool to Help Speed Liver Disease Drug Development. December 9 2025. Available at: https://www.reuters.com/business/healthcare%2Dpharmaceuticals/us%2Dfda%2Dqualifies%2Dfirst%2Dai%2Dtool%2Dhelp%2Dspeed%2Dliver%2Ddisease%2Ddrug%2Ddevelopment%2D2025%2D12%2D09
[22] Insilico Medicine. ISM001 055 Was Safe and Well Tolerated with Favorable Pharmacokinetics and Encouraging Clinical Efficacy in Phase IIa Trial. November 2024. Available at: https://insilico.com/news/tnik%2Dipf%2Dphase2a
[23] Mahalo Health. AI in Clinical Trials: Use Cases, Trends, and What Comes Next. June 2025. Available at: https://www.mahalo.health/insights/significance%2Dof%2Dai%2Din%2Dclinical%2Dtrials
[24] United States Food and Drug Administration. Artificial Intelligence at FDA: Publications. March 2024. Available at: https://www.fda.gov/science%2Dresearch/artificial%2Dintelligence%2Dand%2Dmedical%2Dproducts/artificial%2Dintelligence%2Dfda%2Dpublications
[25] Covington Digital Health. FDA Medical Product Centers Continue Focus on AI. April 2024. Available at: https://www.covingtondigitalhealth.com/2024/04/fda%2Dmedical%2Dproduct%2Dcenters%2Dcontinue%2Dfocus%2Don%2Dai
[26] Reuters. US FDA Centers to Deploy AI Internally, Following Experimental Run. May 2025. Available at: https://www.reuters.com/business/healthcare%2Dpharmaceuticals/us%2Dfda%2Dcenters%2Ddeploy%2Dai%2Dinternally%2Dimmediately%2D2025%2D05%2D08







